Hi, welcome to another episode of Unlocked. I am Skot and today we're talking about unlocking the potential of patients, not just people. Well, of course people are patients or patients are people, I guess we should say it that way. Today, Dr. Talya is on the call and she lives at this really, really interesting space of behavioral economics and decision making and healthcare. And she lives in this really cool space, right in the middle of those two and works every day with healthcare industries to market, to talk about behavioral change, to do research. She does a ton of research. She knows her stuff. She just released a new book and we're going to talk all about that in this interview. You're also going to hear some awesome guidance about decision making and as a patient, how you can unlock your own potential to receive the best healthcare possible.
And I don't care if you're anti-vax, pro-vax, I don't care if you are Republican, Democrat. I don't care if you're anti-pharmaceutical, pro-pharmaceutical, whatever your viewpoints are, and Talya makes hers pretty known in this interview. I don't think she's trying to hide them but the message is clear and applicable to everyone. This book is applicable for everyone and she talks about that at the end of the interview. We have this great message and she has this little monologue that she has that's awesome. That's really, really powerful so I hope you'll take some time to listen to that. Let's get on with the interview. Here we go.
Dr. Talya, can I call you Dr. Talya? Is that safe?
Dr. Talya Miron-Shatz:
Yes.
Skot Waldron:
That cool?
DR. TALYA MIRON-SHATZ:
It's very safe. Talya with a Y, yes.
SKOT WALDRON:
Okay, yes. Yes, yes. Dr. Talya, good to have you on the show today. Appreciate you being here and your new book, Your Life Depends on It, just launched and I would love for you because I've seen this book all over the place, in my LinkedIn network. We belong to a small group there and I've seen it everywhere. I've read a small snippet of the beginning and I would love for you to share with the audience where that idea came from, why are you writing this book? Our Life Depends on It is a pretty bold title. Tell us about that.
DR. TALYA MIRON-SHATZ:
Well, it is but that's also true. It's called, Your Life Depends on It: What You Can Do to Make Better Choices About Your Health. And the idea is that we make health and medical decisions all the time. If people did not believe me until now, COVID came and made that very, very clear. And it's also pretty clear that sometimes make decisions that don't benefit our health. Now that's really unfortunate and sometimes it's in big way, sometimes it's in smaller ways. I've been working with health and with decision making for almost 20 years now. I have a PhD in psychology, so I do a lot of research on medical decision making and I taught about it. I taught at Wharton and I did research at Princeton. I'm a visiting researcher at the University of Cambridge so there's a lot of academic credibility behind that but there's also a lot of industry involvement and I've been working with pharmaceutical companies and health advertisers and developers and whatnot because I think it really is important to bring all this knowledge into implementation, into action and help people do a better job.
By people, I mean all of us. I mean you and me and people who are much less educated than us and people who are much more educated than us, medical professionals, basically everyone because you probably know this, behavioral economics has become a major field now. Everyone has read the books, Daniel Kahneman, who I worked with, and Richard Thalor and you've read Nudge and the works and Dan Ariely of course, everyone's read that. What I do is I take this knowledge and I implement it to health, to medical decision making. Which is a place where no one has gone before and they should because every bit of bias that we always have applies to our health. And guess what? That's pretty dangerous.
SKOT WALDRON:
That is. We do make decisions about our health every day. It's applicable for all of us. Saying that, you mentioned, we make decisions about our health every day and sometimes not so great ones. What are those not so great decisions that we tend to make about ourselves where we should maybe be more mindful?
DR. TALYA MIRON-SHATZ:
Let's talk about the process by which we make a decision. We have two ways of thinking. We have system one and system two. System one is quick and dirty and it's like how you grab a stand, you grab. It's quick. You just go for something. You say, "I feel like it." That's it. Very quick, very little input goes in there and a lot of emotion. System two is where you really think and you really ponder and you really process a lot of data but that's also very hard. When we're talking about, say medication, can you really read the brochure and the related papers, et cetera? Maybe you can, maybe you can't.
And in fact, in the intro to my book, I talk about a case where I, the medical decision making expert had massive backache and my doctor initially gave me nothing. Then he said, "Oh, here's a morphine patch, it will help." Dude, a morphine patch? Are you kidding? Are you moving from giving me nothing to a morphine patch? Do you think I said that? I did not. My system two, of elaborate thinking was what was it? It was asleep. It was sore. I was in pain. I wasn't thinking. All I could think of was pain relief, please. That's it. And that didn't go so well, actually. That's just one example.
In other cases, people say, "Oh, I just want to go with something natural." That's commendable but the good old days when we lived in caves, if you had the tooth infection, it could kill you. Do you only want to do things that are natural? Do you only want to go by this one word label? Or do you want to probe a bit deeper? That's the kind of question we need to ask. In the context of vaccination, I'm not going to say what my opinion is, you could probably guess but some people are saying, "I don't want to put anything in my body." Well. Well, well, guess what? Have you ever had Coca-Cola? Because that's a form of chemical as well. Or hot dog. Let's think about this a bit more deeply. That's on our side as consumers and the flip side of that is as advertisers as educators, let's help people think about this, if not more deeply because that's hard, more effectively to do better by their health.
SKOT WALDRON:
What do we do about that decision making process? Because there are many of us that are fed from emotion that is going to say, "I want immediate relief. I feel immediate pain, I need immediate relief and this is an emergency. I feel fearful." Because our health, it's a scary thing. Fear drives a lot of decision making. We use it when I used to do a lot of marketing for companies and organizations, selling products and services, fear based messaging is part of that at times. What happens if you don't find a solution? What happens if you don't this? And to think about that. Sometimes we don't like to think about that. How does that feed into the decision making process with our health to make sure that we're doing things based on the benefit and not always out of fear?
DR. TALYA MIRON-SHATZ:
That's a really great question. It's one of the reasons is why I wrote the book. I wanted people, not sick people, it's not the book to read when you're sick. It's the book to read when you want to empower yourself, when you want to learn how to hack your health. We have to have the skills for probing a bit more and I say a bit more because I don't expect everyone to now become an MD. We need to overcome our desire for certainty because there's very little certainty in life and when someone guarantees a solution, hmm that's you should become skeptical because can they really guarantee a solution? Is there really certainty involved? I think that's part of the thing that are very difficult for us right now around COVID is that there's no certainty and it's really it's a case that's happening on a rolling basis. The knowledge that we had a year ago isn't the knowledge that we have now.
You have to have trust and that's a first thing. We spoke about emotion. Emotion is definitely a major part of trust. You have to figure out who do I trust around this? Who is going to give me information that is valid and not biased? And that's a major decision before even looking at the information itself. When we're offered things, as you said, marketers, do that all the time. Guilty as charge, I work for their advertising industry as well. On the prescriber side also interestingly, also, as I said with doctors because they're human. When we're offered something, it's really tempting to say, "Oh, it's going to alleviate my fear. It's going to give me hope."
It is very important to ask, "How many people will actually reap the benefits you're describing?" Because sometimes it's few people. Sometimes it's not everyone who will take the drug or try the procedure or sometimes it's half. Sometimes it's fewer. Interesting, so the picture's a bit complex. We don't like complexity but we should be able to look it in the eye and figure out what to do with it. Otherwise, we're falling for the, I don't want to say a marketing scheme. We're falling for something that we hope will give us things that it may not be able to give.
SKOT WALDRON:
Okay. Let me ask you this question because I'm curious about this. In my experience in working with CDC many, many years, we talked a lot about gain frame messaging versus loss frame messaging. The principle of if you don't stop smoking, you will get cancer and die. Loss frame. Gain frame is if if you stop smoking, you will be around long enough to see your grandchildren grow up and get married, whatever. Which one in your experience is most effective in the space and with the science and the data that you've analyzed?
DR. TALYA MIRON-SHATZ:
Right. It goes back to prospect theory by Daniel Kahneman and Amos Tversky. And what they showed is that losses loom larger than gains. To lose something is more meaningful to us than to gain something. You lose 20 bucks, you go crazy. You find 20 bucks, yeah that's nice. There's no comparison there. Basically losses are, will do a better job of driving us but you need to caveat this in a number of ways. And one of the ways it needs to be refined. With fear messaging, if you scare people too much, they just avoid the message altogether. And you see on cigarette packets, you sometimes see very scary pictures so what do people do? They just look away. They're still going to buy the cigarettes. They're just going to ignore your scary messaging because it is too frightening. There's a limit there also to what you can do.
And likewise, with the rewards, you're saying, "You see your grandkids get married." You know what? I wish I had grandkids. I don't have any grandkids yet. I don't smoke either. But if I don't have grandkids and you're selling me something that's so far and intangible, it may not be experienced as a gain. And that's actually a major issue with preventative medicine because what you're telling me, you're telling me, "Look Talya, quit smoking, quit drinking, start exercising, start taking pills." I will look at you and say, "Skot, what do you want? You're just making my life a misery." That's actually really not me. I get drunk on nothing and I don't smoke and I exercise anyway. But if that were the case, I would say, "I don't know, you're taking all the fun out of my life and for what? It's a bit of a pie in the sky that when you grow older, whatever, it's not convincing."
That's a major challenge for us behavior change people and the CDC and physicians and advertisers to find the psychological, the behavioral economics mechanism by which to drive people to doing the right thing repeatedly, continually, even when there's no immediate reward. Let me give you a very bold medical example. People who have atrial fibrillation need to take medication. With atrial fibrillation, you don't feel the symptoms. It's as if you don't have a problem. You're taking medication and it's kind of presumably helping you solve the problem that you never felt you had. There's no problem and there's no benefit to the medication. And a lot of people say, "I'll just quit with with the medication, if there's a problem I'll continue." Now guess what? The problem is that you get a stroke. That's not something anyone wishes to experience.
This line of thinking is very natural to people. It's not serving them well at all but if you're a physician or a marketer or the CDC or Humana or Aetna or any of those insurers, you have got to create the mechanisms that will convince people to do the right thing even if it feels useless or even annoying in the short term.
SKOT WALDRON:
How do we build enough trust? Because you mention this in the book, you're going through the book and you talked about your story at the very beginning of your back. And so I want you to hit on that briefly about that story and that experience because I think that adds some context to the discussion. And then talk about, you mention in there, the difference between us now, access to the internet versus then when you were a child and there was no internet, you trusted your physician. They went to school, they had letters behind their name and you just said, "I'll do whatever they say because they're smarter than me or they are supposed to know best." Hit on that experience as you were a child and then how that shaped up this dialogue between what we know now in building trust versus what we knew then and just trusting blindly.
DR. TALYA MIRON-SHATZ:
Absolutely. I think what we did in the past was we lived in a paternalistic model where the doctor said something and you just followed because that's what you were supposed to do. And things have shifted. Things have shifted because we now live in more of a consumer driven world and we expect to have that also in our medical care, we have a lot more information. I was completely ignorant as a kid and there was no internet and there was nothing and I didn't even know where to go looking for information. I'm first generation in my family that went to college. I didn't know there was a university library or how to get in there at all. How to look for anything. In this day and age, things are very different because we have a lot of information that's accessible to us.
In theory and sometimes we think we can make medical decisions or we think we have more agency in our care and that's in theory. Great. What I wrote about out is that we also need guidance and I actually wrote a piece for the Wall Street Journal and that got a lot of traction because some people were very angry with me saying, "We need help making medical decisions." Some people said, "What do you mean? I don't need help." Well, maybe we don't need help but a lot of people do. And even though we experience this as an individual difficulty, it's something that needs to be taken care of at a systemic level.
When I was a kid and I had a doctor who barely spoke to me, never asked me if I had any questions or never explained anything or never gave me any information, I experienced this as something that went on between me and her. Now I understand many years later that yes, it happened between me and her but it happened within a medical establishment that did not care about me having a connection with her or having a place to ask questions or to be a bit more of a consumer, to be a bit more informed about what was happening to me. That's definitely one piece of it. And a word you mentioned repeatedly because it is so crucial is trust. If you don't have trust, you don't have anything. That's astonishing actually, when you think about it in the medical context. If people don't trust their doctors, they don't follow up on what their doctors say and ask them to do.
You could say, "Come on, that's really stupid because who are these people punishing?" They're actually punishing themselves their own health. Yes, that's true. But they're doing it because something isn't working in the relationship and it's phenomenal because it also translates to digital health. It translates to any relationship or seeming relationship that we have with a device, with an insurer, with anybody. If you don't establish trust and I do that when I work with digital health developers, if you don't establish trust, you have nothing. And after trust come other layers of conveying information in ways that people understand. Because if they're consumers, let them actually be consumers and know what they are consuming and have some say in the matter. Then creating choice, et cetera. It's layer upon layer. But without trust, that's the basis of the pyramid.
SKOT WALDRON:
How do demographics or psychographics or generational makeups fit into this whole model? Because I bring this up because my dad, 82 year old, middle class, he still works.
DR. TALYA MIRON-SHATZ:
Wow.
SKOT WALDRON:
As an accountant. I call it working. He'll wake up, he'll go into work at 10:00, he comes up at 2:00 and takes a nap. It's kind of a nice hobby now. But what I'll say is that we, meaning us children, can talk to him about his health all we want. Very conservative, tips that are out there for the whole world and he shrugs them off, "Meh, yeah. That's okay. I'm not going to do that. Oh, I'm almost dead anyway." All these comments that old people say. If his HMO doctor says, "Bob, jump," he jumps. "Bob, take this pill," he takes the pill. "Bob, you should get the surgery," gets the surgery like clockwork. He will do anything his doctors tell him to do. And we sit there and go, "Dad, hold up. You should probably think about what he's asking you to do. Take it for sure but think about that a little bit." Talk about that generational gap. Talk about the demographic psychographic of healthcare decision making.
DR. TALYA MIRON-SHATZ:
Of course. And I love that you ask that because if we ignore that, we're just pretending we're all the same. We are not. We're equal. That doesn't mean we're identical because we are definitely not. I believe your father belongs to a generation that deferred to doctors, that grew up on the paternalistic model where the doctor says something and Bob just does it because the doctor said. And I bet if you said, "Well Dad, did you ask about alternatives?" He would say, "Skot, what are you talking about? Did you go to medical school? No. And I didn't either. This is what the doctor says and that's the best thing for me."
Generationally speaking, we now live in a different generation. We have access to much more information. We are less deferent. We're more likely to ask for alternatives and to probe and to bring more information into the treatment room. Now having said that, I want to caveat it in two ways. And one of them is actually quite surprising.
I want to go back to digital health and to tell you about a study I did with colleagues where we looked at people who were 75 and above and never held an iPad in their lives, tablet, anything, an iPhone. We gave them an iPad and they used it for medication adherence and they absolutely loved it and it increased their adherence. What was the secret? There's the secret here? Because you can't assume that by creating great digital health opportunities, you're serving the entire population. We actually navigated it for them. We brought it to their homes. We put a sticker where you turn on the iPad because if you've never held one and you're 75, it's not intuitive to you. It's just confusing. We did that and we muted everything else on the iPad and we just programmed for them their medication names and they loved it.
What does it say? It means you can bring digital capabilities to multiple places but you have to bridge them for people. You have to help them into it. You have to ease them into using this device, otherwise you're just pretending. You're throwing something at them that they don't know how to use. But that's, for me, it's also a very encouraging message because it says people shouldn't be excluded but we also shouldn't just assume that they're going to use whatever you and me or our kids can use just the blink of an eye. That's one thing.
There are other places where we can't assume that everyone's the same. Some people are more different than others because they don't feel as entitled. They don't feel as educated. They don't feel they have as much standing in the world and they're less likely to stand up to a doctor and some people are discriminated against. And it can be unintentional but there's a lot of implicit bias that goes on when a White man, like you goes into the ER and complains of pain. The doctor says in their mind, here's a White man. As I know, all White men are strong, silent cowboys and if they complain of the pain, that means they're in pain and they should receive pain medication. Cool. If you're a Black man or a Hispanic man and you complain of pain, that's a different story and you have to wait much longer to receive the same pain medication with the same injury. Now that is a very harsh reality.
What do you do? What do you do? Also, if you belong to a minority that I happen to belong to of women, 51% of the population, well we all know that women are hysterical and if they complain of something, it's all in their mind and it's psychological. That's sometimes is what we get and it's hard to combat. It really is because if you confront your physician about that, it may not go very well. What I think we can do and I think we can do things on two levels. First, I want to go to the system level, that's above my pay grade. You can't do it. I can't do it. Healthcare executives, I hope you or listening fellows and ladies, because it's on you. There need to be protocols built in. If I'm complaining of pain at a certain point in the scale and a White man is, we should be treated the same way. There of course needs to be room for the doctor's consideration but there also have to be good defaults to make sure that people are not discriminated against. That's something that should happen at the systems level.
Something that we can do as individuals is to ask questions. Politely, you don't want to have a fight with your physician but you could ask if you are not being given pain medications, "What's the standard protocol in this case? What's happening because I'm experiencing a pain, a level of eight, you just amputated my knee," or I don't know what, "and could you help me? What do you usually do in these cases?" And that can help our physicians get out of the mindset of saying, "Oh, this person belongs to a minority. They're just complaining." As opposed to, no, they're strong White man and therefore they're in pain. And say, "Well, you know what? With a pain level at eight and having just amputated your knee." Of course, that's a crazy example I'm just making up, "I have to give you something for your pain." That's creating a rule.
And I have another tactic for women to use or basically for anybody when you get told that what you're experiencing is psychological. They love that, psychological. You have pain, your doctor can't help you and they're telling you're nuts. That's just wonderful. I propose asking, "Could there be another medical explanation?" That opens it up. That reminds the doctor of where they're coming from. They come from an evidence based place with a lot of medical knowledge and let's put that good knowledge into use because saying it's psychological is saying, "No, I don't know. I'm not going to probe any further. I'm going to leave you to it." And by now that is unsatisfactory.
I wrote Your Life Depends on It: What You Can Do to Make Better Choices About Your Health and I wanted to empower people but I also wanted them, us, to understand the limitations of our empowerment because we are patients within systems and there's only so much we can do there. We have to understand that or otherwise we would be incredibly frustrated and even disappointed at ourselves for not being able to accomplish more.
SKOT WALDRON:
Well said. Well said. I think what you said goes along with a principle I teach of moving from critique to curiosity. If we feel we're being treated unjustly in some way, shape or form, instead of turning and just ranting and complaining and throwing the book at this person and then going to whoever, it's you pose a question. You moved onto, is there another medical explanation for this? Beautiful. Moving to curiosity, as opposed to just critiquing and complaining all over the place. I think that that's really great insight that you can share with anybody and everybody should take that away.
How do we, in this context, in the digital era of mass information, some good, some bad, we believe what we're going to believe because of confirmation bias. That plays a huge role into it. We're affiliated with religion, we're affiliated with political beliefs, we're affiliated with economic status and what we do and what we see. And we have our beliefs about certain things. Some of us believe that corporations, pharmaceuticals, the government is out for themselves and it's corrupt and we shouldn't believe anything they say. Some of us are full on, we believe wholeheartedly in what they're doing, they mean well, they are trying to do the best for mankind. Make sure that we all operate as a good running system. There's some stuff in there. We get it but all in all, they're on the up and up and we should really give them the benefit of the doubt. What do you say to those two camps of people?
DR. TALYA MIRON-SHATZ:
I say, first of all, do good by your own health. That's the most important thing. If you're following a political leader and what you're seeing is that people are dying of something that could be avoided, maybe they're the best political leader in the world but is that really what you want for yourself? Do you really want to put your body, your family in danger? I'm not sure. I'm really not sure. Politics, I wrote an article, I called it, Get Your Politics Out of My Pandemic. If only we could do that. Politics is a place where people have various interests and your own health isn't always their top of mind. And that's fine as long as you realize that and you recognize that. Everyone has an interest. Pharmaceutical companies are there to make a buck. Yes, that's true. They are companies for a reason. They are publicly traded et cetera.
Does that mean they all lie all the time? Really? Because when you have an infection, I think you want to get antibiotics and it's a pharmaceutical company that manufacture them. If you demonize them, what are you left with? Turmeric and lemon juice? I don't know. I want to have a bit more than that in my arsenal. I think we need to be adults in the sense that we need to be critical of whoever is giving us information. We need to understand it. A lot of the people who are speaking to us will have interests that might be different from ours. And we need to think, how am I benefiting myself and my body and being responsible and being really critical of information that I receive? And trying to find evidence that does not agree with it.
If I think masks are useless or vaccinations are useless, I should look at disease rates and say, "Oh my God, wow. People who are unvaccinated are much more likely to catch COVID and to die of COVID. Hey, in many states I can see that. That's not great. Why would I put myself in that camp where people are dying? I don't want to be there." Regardless of my views, of my political views, please, to the degree that we can parse our politics from evidence, I think it will only do a good. It's too easy. It's like I said about system one, to say, "I follow this person no matter what they say, no matter the consequences to my health," that's a big thing to say. Am I willing to say that about someone and put my family in jeopardy? I don't know.
SKOT WALDRON:
I have friends on both sides of this camp as we all do. And I would say on the other side that those people would say, you've got the one side of saying, "Why would you jeopardize yourself?" on that side. But I would hear the people on that other side saying, "Why would you jeopardize your health?" on that side, "Why would you follow that political leader?" If we're going to take that political. It has become very political. It's not going to go away. It's a very political thing. And I would say out of this context of you're going to have, they both believe what they believe. They both believe what the other person believes just at the other person. That's what makes it a little bit confusing and hard because it's an inner belief system that you're messing with here. Data is not emotional.
DR. TALYA MIRON-SHATZ:
No, it's really not.
SKOT WALDRON:
And so people make decisions, irrational or rational based on belief systems and emotion, not based on data. And I know the CDC doesn't necessarily like to hear that. We use the data to inform us but we're going to find confirmation bias. We're going to debunk the data because we don't believe that that supports our viewpoint. Where do we go from there? When we're talking irrational behavior and one way from either side of the fence, how do you deal with that when data doesn't really resonate?
DR. TALYA MIRON-SHATZ:
Data doesn't resonate. I could say that to the CDC. I could have a speakerphone just screaming that to the CDC or the City of New York that is trying to do a really good job at bringing an African American doctor to talk to people about vaccinating and I see for flu and for COVID and I see that every day on TV. The more you speak as a government agency, as an insurer and you cater to people's system logic, their emotional beliefs, the better you are at convincing them. That's the truth. That's the level at which we need to speak with people in order to engage them and in order to convince them. And the better we get at that, the better job we could do at persuasion. That's something really to remember with every kind of messaging, including to prescribers. And what we can do as consumers is to try and tolerate that ambiguity, that uncertainty, to understand that they're there to stay.
People are asking about vaccinations, what are the long term effects? We don't know. We only know effects for about two years or under because that's how long these vaccinations have been around. What's the alternative? We could just hold off on vaccinating anyone and look for 15 years data. But what's the world going to look like with 15 years of COVID? That's the place where we need to withhold and we need to say, "That's as good as evidence as I'm going to get and I'm either going to go with it or I'm not going to go with it." But it's not nothing that gives me certainty at this moment is going to be available, there's just no such thing.
SKOT WALDRON:
The title of this show is Unlocked. It's about unlocking the potential of people. And so a lot of people are going to hear this episode and they're going to go, "Wait Skot, you usually talk about leadership and team communication and unlocking humanity through unity and whatever. Some bigger concepts." What would you say is the message here for everyone? That what do we need to unlock right now in all of us, in order to meet our full potential?
DR. TALYA MIRON-SHATZ:
In order to meet our full potential as patients and as people who take great care of our health, we need to learn the skills to help us get there. We to learn to ask questions about risks and benefits and alternatives, it's simple. What are the risks? What are the benefits? What are the alternatives? That can help unlock your potential to be a smart, empowered consumer when you're sitting in that examination room and you're in pain and you're anxious. That's the type of information that you need in order to unlock that. And when I speak to healthcare executives, when I give talks to them, it's like, they're not there to sit back comfortably and wait for dinner. They're there to listen and there's homework because they have to help people, people being both doctors and patients, unlock their best patient potential. It doesn't always happen on its own. That's important. The message of empowerment, the message of unlocking is great but it has its limitations. We need help and that's why we need everyone in the healthcare system to jump in and participate.
SKOT WALDRON:
Beautiful. Beautiful, beautiful. Your Life Depends on It, it's out now. Where can people get a hold of that?
DR. TALYA MIRON-SHATZ:
Everywhere where books are sold, Your Life Depends on It: What You Can Do to Make Better Choices About Your Health by Talya Miron-Shatz, Talya with a Y. If you look for more information, there's a ton of it. There's a lot of free resources and webinars on health inequities and nudges and whatnot on my website. That's taliamironshatz.com, T-A-L-Y-A-M-I-R-O-N-S-H-A-T-Z.com. There's more information on the book there and there's really plenty to read for anyone who's super interested in making better medical decisions.
SKOT WALDRON:
Very cool. Awesome talking to you today. I'm glad we finally got to interact in digital person. This was fun. Thanks Talya, for being on the call and good luck with the book.
DR. TALYA MIRON-SHATZ:
My pleasures, Skot and thank you so very much for this opportunity.
SKOT WALDRON:
Did you learn a little something in there about making decisions, just decisions in general? It was really insightful, some of the things that she said. I love that message about the psychology of loss frame versus gain frame. The fear is going to override the gain most of the time. And I know we don't like to think that and believe that but it's true. We're much more likely to do something to avoid pain than we are to achieve gain. And that drives a lot of our healthcare decisions. A lot of that fear inside of us, a lot of that fear about our future, that fear of what's happening to me right now, drives a lot of those maybe irresponsible healthcare decisions and we should take a moment to do what Talya says, ask questions.
Be curious. There are alternatives. Most of the time there are alternatives and it's your responsibility to ask about those alternatives. It's your responsibility to be informed about what you're doing to your body for your own benefit and for the benefit of your family and the benefit of everyone around you. Society in general. We want to make sure that we are giving the benefit of the doubt to the people that are taking care of us. We hope that they're doing it out of goodwill and we hope that they're doing it in order to help us all become better. We hope that they all went to school in whatever medical profession they're in, to help people be better. If they didn't I hope I don't have that doctor. The ones that I do have, I want to believe in and I want to believe that they're there for me but it is my personal responsibility to inform myself as much as possible. And I know it's hard. Talya says it's hard. It's not easy but it's our responsibility to do so.
Thank you, Dr. Talya for being on the call. Good luck with the book launch. If you want to find out more about me, you can go to skotwaldron.com. You can go to my YouTube channel, like, subscribe, comment there. There's a bunch of videos, a bunch of educational content that's free for you and you can also find me on LinkedIn. I'm there a lot. Thanks everybody for being here. Hope you learned something on this episode of Unlocked.
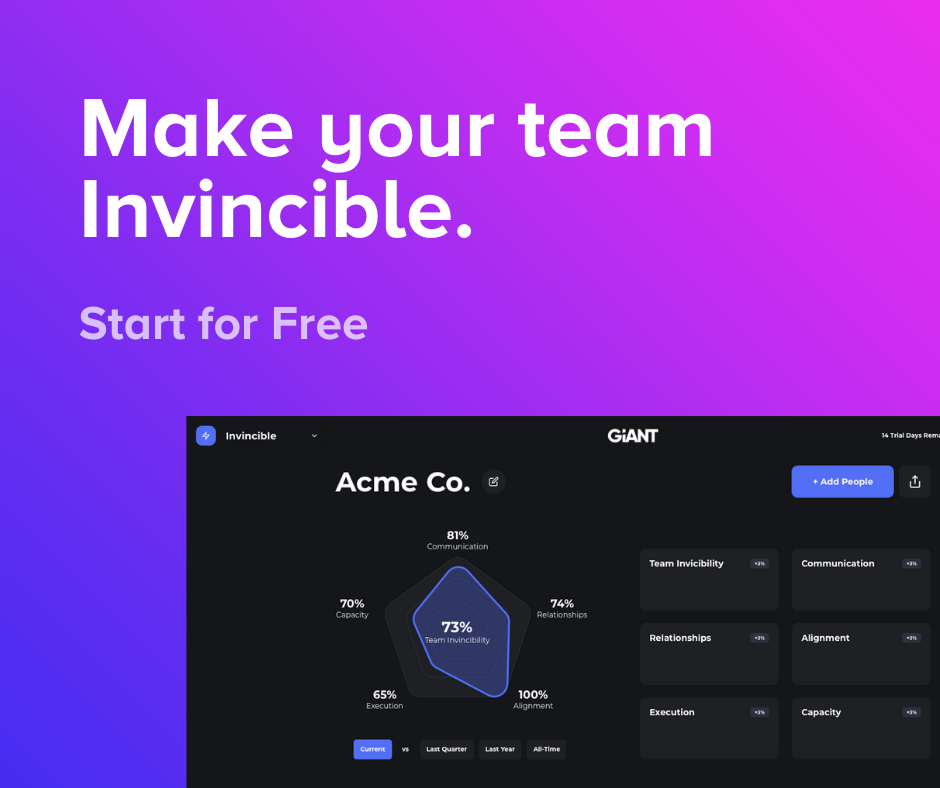
Want to make your culture and team invincible?
You can create a culture of empowerment and liberation through better communication and alignment. We call these invincible teams. Make your team invincible through a data-driven approach that is used by Google, the CDC, the Air Force, Pfizer, and Chick-fil-A. Click here or the image below to learn more.